Angiokeratoma of Fordyce
Angiokeratoma of Fordyce is the most common type of angiokeratomas and occurs in the genital area. Angiokeratoma of Fordyce is not contagious, sexually transmitted or cancerous.
Although they are usually asymptomatic and typically do not require any active intervention, troublesome intermittent bleeding from the papules can be an issue for some patients, necessitating the treatment of these lesions.
The angiokeratomas do not disappear on their own but need treatment to go away.
Symptoms of Angiokeratoma of Fordyce
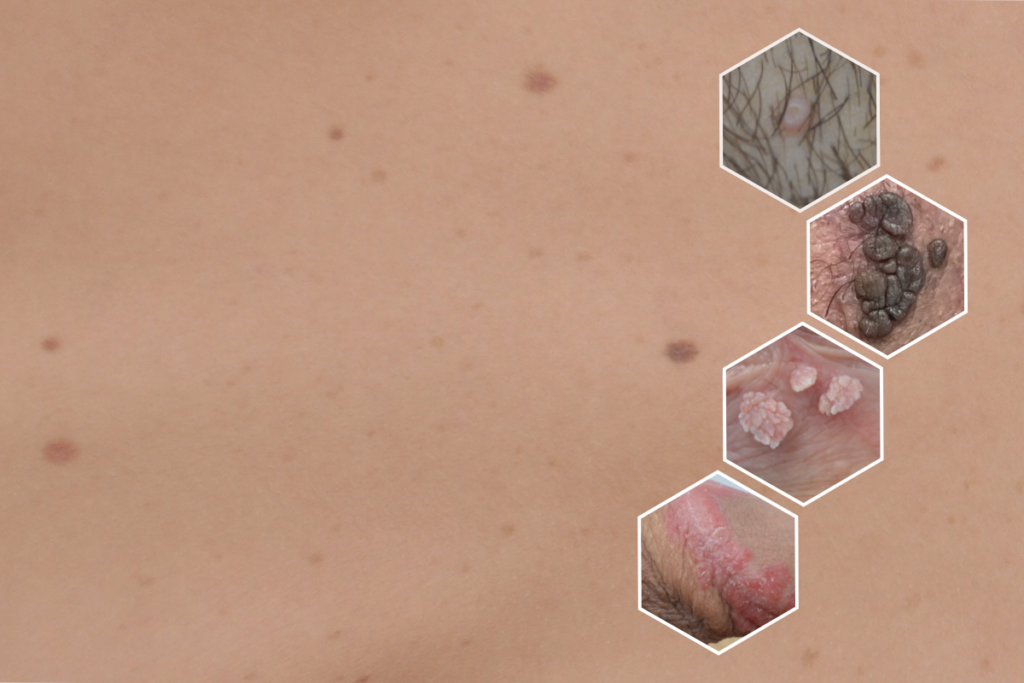
Angiokeratoma of Fordyce appears as spots in the genital area, ranging anywhere from dark red to purple, or almost black in colour. Most commonly they appear on the scrotum, but they can also appear on the vulva or on or around the penile skin. Most patients tend to have lesions between 1-5mm in size but much larger lesions can be seen in more advanced cases where lesions may be large enough to look like warts. The angiokeratomas may show up individually or in clusters and the papules often have tiny visible capillaries connecting the larger blood filled lesions.
Most patients do not feel any discomfort from the angiokeratomas, however, some patients may feel a bit of discomfort accompanied by a sense of warmth and itching. They tend to bleed if traumatised or accidentally cut during shaving or trimming.
Some patients can have angiokeratomas, skin tags and genital warts all at the same time. If you are unsure what lesions you have, seek medical advice for the correct diagnosis.
If the Angiokeratoma of Fordyce is the result of an underlying condition, such as Fabry disease, other symptoms may be present. These symptoms include pain in the upper and lower limb extremities, tinnitus (a ringing sound in the ear), lack of sweat (hyphohidrosis), cloudy vision, or lower abdominal pain.
Causes of Angiokeratoma of Fordyce
Angiokeratoma of Fordyce can occur when blood vessels near the skin’s surface break or dilate, causing a bump on the skin. A common cause for this is when the supporting tissue around the capillary walls loses its elasticity.

Prognosis of Angiokeratoma of Fordyce
There is no need to worry as it is a benign condition and does not lead to cancer.
Get Tested with Confidence
Consultation
Testing
Treatment
Frequently Asked Questions
What areas of the genitalia can Angiokeratoma of Fordyce affect?
Angiokeratoma of Fordyce can occur anywhere on the genitalia but commonly occur on the scrotum and the vulva. They are seen less commonly on the glans penis and penile shaft. Other types of angiokeratomas can occur elsewhere on the body, but Angiokeratoma of Fordyce is only present in the genital area.
Whom does Angiokeratoma of Fordyce affect?
Anyone can develop Angiokeratoma of Fordyce. Most people with these lesions have no underlying medical problems. It most commonly affects patients that are 50 years old or above, and it is more common in male patients.
Can Angiokeratoma of Fordyce go away?
Angiokeratoma of Fordyce does not go away on its own. They can, however, grow in number overtime.
What complications can Angiokeratoma of Fordyce lead to, if untreated? K L
In most cases, Angiokeratoma of Fordyce present on the skin does not progress to anything serious. It is not sexually transmitted or contagious, and does not cause cancer.
Troublesome intermittent bleeding from the lesions can be an issue for some patients, necessitating the treatment of these lesions.
Can you get Angiokeratoma of Fordyce in a different area of your body? K
You can get other types of angiokeratomas in different areas of your body, but Angiokeratoma of Fordyce only occurs in the genital area.
Is Angiokeratoma of Fordyce an STI, and/or is it an infectious disease?
No, Angiokeratoma of Fordyce is not an STI, and it can not be transmitted to someone else through sexual contact. Angiokeratoma of Fordyce is also not cancerous.
How is Angiokeratoma of Fordyce routinely diagnosed?
Typically, a diagnosis can be made by a visual examination. However, in the event of bleeding or other concerns, the doctor might take a small tissue sample called a biopsy to examine under the microscope.
Can another condition be mistaken as Angiokeratoma of Fordyce?
Angiokeratoma of Fordyce may be easily mistaken as other conditions, such as:
- Genital warts
- Genital herpes
- Molluscum contagiosum
- Skin tags
- Skin inflammation (folliculitis)
- Other benign skin conditions such as milia (hard bumps on the skin due to the build-up of keratin)
- Basal cell carcinoma
If you are unsure whether you have Angiokeratoma of Fordyce, particularly if the lesions are newly visible, it is important to see a healthcare professional for an accurate diagnosis.
Is there any other way to diagnose Angiokeratoma of Fordyce?
Unless there is diagnostic uncertainty, confirmation beyond an examination by your clinician is not normally required.
Can I request a second opinion about my diagnosis?
Of course. We understand that you may wish for a second pair of eyes to assess your condition. You are more than welcome to book an appointment with another clinician as well – either at our clinic or elsewhere.
Does Angiokeratoma of Fordyce require treatment?
Angiokeratoma of Fordyce is not harmful and typically does not require any active intervention.
However, some patients want them removed for cosmetic reasons. Some patients find that the angiokeratomas negatively affect their confidence. We have seen many patients whose lives are greatly affected by these lesions and for some it is difficult to build and maintain relationships.
Sometimes patients prefer sexual intimacy with their partner(s) in darkness, due to the presence of these lesions. In these cases, a simple procedure can help patients to regain confidence and rebuild their life.
Once treated, will I be able to develop Angiokeratoma of Fordyce again? K L
Lesions may recur years later in the same or different areas.
How can I prevent Angiokeratoma of Fordyce in the future?
A common cause for Angiokeratoma of Fordyce is that the supporting tissue around the capillary walls loses its elasticity. Because this can be genetic there is no specific advice for how to reduce the risk of recurrence.
Do I have to tell my partner I have (or have had) Angiokeratoma of Fordyce?
As Angiokeratoma of Fordyce is not infectious or sexually transmitted there is no implication or concerns for your sexual partner(s). There is no requirement for you to share your diagnosis with your partner(s). Your partner(s) will also not require any treatment.
Author:
Page reviewed by Ms. Magdalena Nowacka
Page written by Shannon Abraham
Last reviewed date: 13 June 2023
Next review due: 13 June 2026
Whilst this content is written and reviewed by sexual health specialists, it is for general guidance only. It is not intended to replace the advice of your clinician.
References & Further Reading
- StatPearls: Angiokeratoma Circumscriptum
- SpringerLink: Penile Angiokeratomas (PEAKERs) Revisited: A Comprehensive Review
- Frontiers in Medicine: Dermoscopic Features Summarization and Comparison of Four Types of Cutaneous Vascular Anomalies
- Hindawi Dermatology Research and Practice: Fordyce Angiokeratoma: Comparison of Cryotherapy and Electrocauterization Treatments
- National Library of Medicine: Fabry Disease


